While type-2 diabetes is largely preventable, type-1 diabetes is a disruptive autoimmune disorder that was once thought incurable. ‘Once’ is the keyword here, as a new and uncontroversial form of stem cell treatment should be able to cure the disease once and for all.
Relying on transforming a small piece of adult skin tissue into beta-cells in the pancreas— the ones which produce the insulin hormone illusive in diabetics—the treatment bypasses the genetic mutation that causes the immune system to attack these cells which creates the disease.
Diabetes, especially type-1, severely limits quality of life, and if not carefully managed can result in serious complications like foot amputations and early mortality.
Furthermore, it costs the U.S. medical care industry around $85,000 per patient per lifetime’s worth of treatment—an enormous burden that if lifted could save the entire sector hundreds of millions.
Researchers at the Salk Institute for Biological Studies, an avant-garde force in all forms biology, have pioneered a new way to produce beta-pancreas cells for this type-1 treatment—and now the only thing standing in the way of it becoming available in a hospital setting is safety trials in humans.
“Stem cells are an extremely promising approach for developing many cell therapies, including better treatments for type-1 diabetes,” Salk professor Juan Carlos Izpisua Belmonte, senior author of the corresponding paper, told the Salk press department.
“This method for manufacturing large numbers of safe and functional beta cells is an important step forward.”
The reason that stipulation is important is that while their paper gives 11 citations to the concept of using stem cell therapy to cure diabetes, going all the way back to 2007, there are challenges, as yet unsurmounted, with manufacturing beta-pancreas cells.
Growing a cure
Before stem cells were used, patients could receive transplanted islet cells from donors with a totally functioning insulin system, but low donor rates made this treatment a slow burner, even though it was successful.
Existing methods of stem cells only successfully convert around 10-40% of the human-pluripotent stem cells (PSCs) into beta-pancreas cells. Additionally, beta-pancreas cells from PSCs tend to be heterogenous and contain unwanted cell types that can impede or disrupt the maturation and function of the desired beta-pancreas cells.
Previous methods for utilizing PSCs to create beta cells also sometimes results in dysfunction, or in some cases the formation of (sometimes enormous) teratomas, or cysts.
“In order for beta cell-based treatments to eventually become a viable option for patients, it’s important to make these cells easier to manufacture,” co-first author Haisong Liu, a former member of Dr. Belmonte’s lab, told Salk. “We need to find a way to optimize the process.”
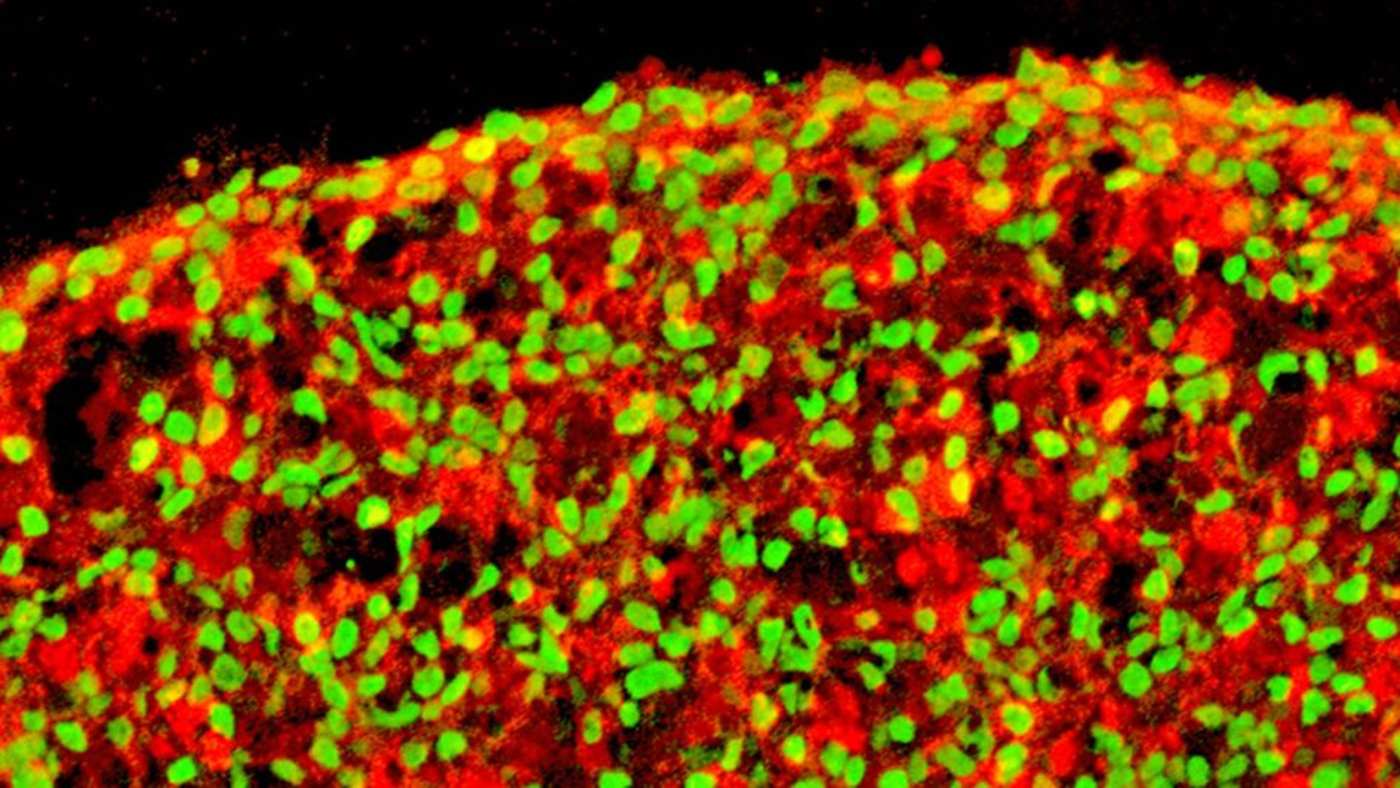
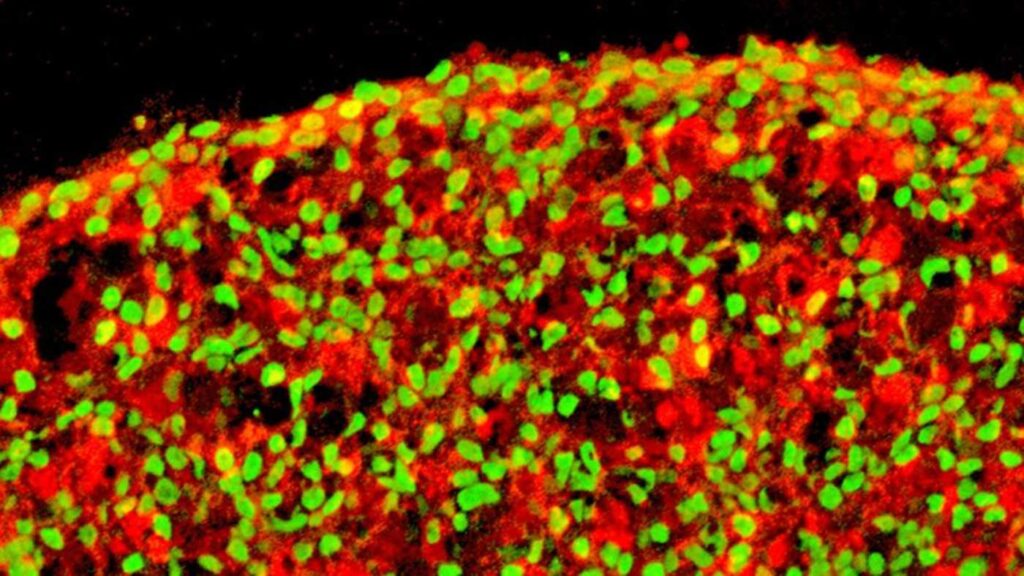
And they did just that. Utilizing a 3-dimensional petri dish allowed the cells to interact and grow in an environment similar to how they would naturally, and within two weeks of being transplanted into diabetic mice, their blood sugars dropped to normal levels like those seen in non-diabetic mice.
RELATED: Walmart Unveils Low-Priced Insulin to Diabetes Patients Who Can’t Easily Afford it
To test the safety and efficacy of the manufactured beta cells, the team transplanted them at different stages and observed the effects. At the highest stages of growth, the cells did not result in cyst formation even 20 weeks after implantation, and exhibited proper functionality in vivo and in vitro.
The method of three-dimensional stem cell production will continue to be refined at Salk, with the only remaining hurdle human trials and FDA approval. At least one pharmaceutical company has already embarked this year on the trials to test a stem cell therapy for type-1 diabetes, so it seems the medical condition’s days are numbered.
SHARE This Hopeful Research With Pals on Social Media…