Engineers at the University of Pennsylvania have made a critical breakthrough that promises better outcomes for pregnancies threatened with pre-eclampsia, a condition that arises due to insufficient blood flow to the placenta, resulting in high maternal blood pressure and restricted blood flow to the fetus.
Pre-eclampsia is one of the leading causes of stillbirths and prematurity worldwide, and it occurs in 3 to 5% of pregnancies. Without a cure, options for these patients only treat symptoms, such as taking blood pressure medication, being on bed rest, or delivering prematurely—regardless of the viability of their baby.
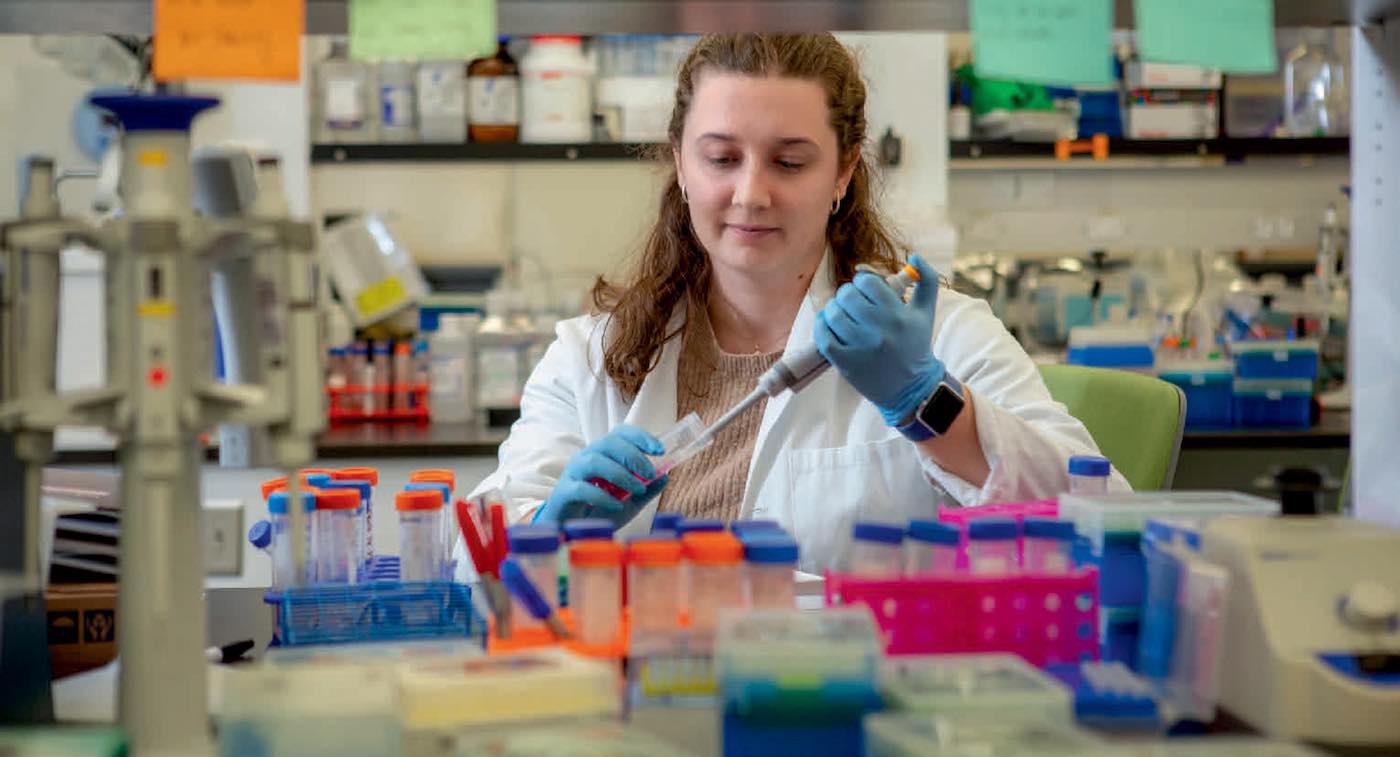
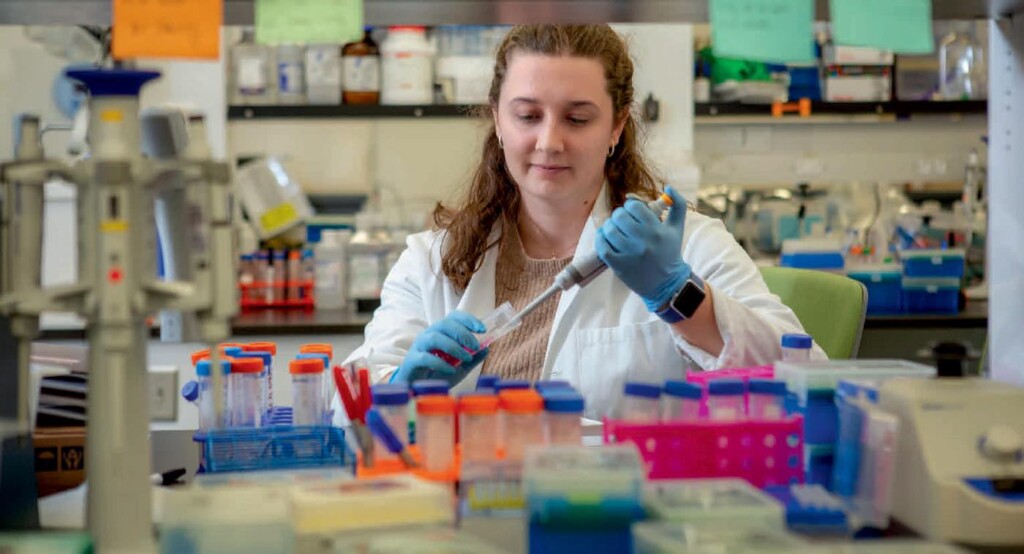
Making a decision to treat pre-eclampsia in any manner can be a moral conundrum, to balance many personal health decisions with long-standing impacts—and for Kelsey Swingle, a doctoral student in the UPenn bioengineering lab, these options are not enough.
In previous research, she conducted a successful proof-of-concept study that examined a library of lipid nanoparticles (LNPs)—which are the delivery molecules that helped get the mRNA of the COVID vaccine into cells—and their ability to reach the placenta in pregnant mice.
In her latest study, published in Nature, Swingle examined 98 different LNPs and their ability to get to the placenta and decrease high blood pressure and increase vasodilation in pre-eclamptic pregnant mice.
Her work shows that the best LNP for the job was one that resulted in more than 100-fold greater mRNA delivery to the placenta in pregnant mice than an FDA-approved LNP formulation.
The drug worked.
“Our LNP was able to deliver an mRNA therapeutic that reduced maternal blood pressure through the end of gestation and improved fetal health and blood circulation in the placenta,” says Swingle.
“Additionally, at birth we saw an increase in litter weight of the pups, which indicates a healthy mom and healthy babies. I am very excited about this work and its current stage because it could offer a real treatment for pre-eclampsia in human patients in the very near future.”
While further developing this cure for pre-eclampsia and getting it to the market for human use is on the horizon for the research team, Swingle had to start from scratch to make this work possible. She first had to lay the groundwork to run experiments using pregnant mice and determine how to induce pre-eclampsia in this animal model, processes that are not as well studied.
But, by laying this groundwork, Swingle’s work has not only identified an avenue for curing pre-eclampsia, it also opens doors for research on LNP-mRNA therapeutics addressing other reproductive health challenges.
“It turns out that there are relatively few studies that have been done with mRNA LNPs in pregnant mice, and little to none done in pre-eclamptic mice,” says Swingle. “Everything is different in pregnancy research. In mice, instead of tracking gestational weeks, we track gestational days so we know exactly how far along their pregnancy is. I had to learn the anatomy of a mouse placenta, and then determine the best ways to establish a mouse model of pre-eclampsia that best imitates the disease in humans.”
CHECK OUT: Molecule in Breast Milk Could Reduce Cerebral Palsy in Infants–By Boosting Brain Matter
In this study, pre-eclampsia was induced in pregnant mice. Then, they injected the LNP with the minimum effective dose once, at day 11 of their 20-day gestation. This one-time injection cured pre-eclamptic mice until the end of pregnancy, but now the team must explore how many doses would be needed to treat the condition in larger animals and humans.
“At this stage in our research, we would bring this LNP to larger animals such as rats and guinea pigs first to determine how well it works in the ‘gold standard’ models of pre-eclampsia before we could advance this work to human trials,” says Swingle.
“Testing our LNP on guinea pigs will be particularly interesting, as their placenta closely resembles a human’s and their gestational period is longer, up to 72 days. We will be asking the questions ‘How many doses do these animals need?’ ‘Will the minimum effective dose change?’ and ‘How well does our current LNP work in each?’”
As Swingle thinks ahead for next steps in her research, which was funded by the National Institutes of Health and the National Science Foundation, she will also collaborate to further optimize the LNP to deliver the mRNA even more efficiently, as well as understanding the mechanisms of how it gets to the placenta, a question still not fully answered.
MORE BREAKTHROUGHS: First of its Kind Brain Surgery on Baby Inside the Womb has Successfully Prevented Heart Failure
They are already in talks about creating a spin-off company and want to work on bringing this LNP-mRNA therapeutic to clinical trials and the market.
Swingle, who is currently finishing up her Ph.D. research, has not only successfully led this new series of studies advancing pre-eclampsia treatment at Penn, she has also inspired other early career researchers in the field as she continues to thrive while bringing women’s health into the spotlight.
ENLIGHTEN CHILDBIRTH PROFESSIONALS By Sharing This on Social Media…