Imagine a world in which a vaccine is a cream you rub onto your skin instead of a needle a health sector worker pushes into one of your muscles.
Even better, it’s cheap, entirely pain-free, and not followed by fever, swelling, redness, or a sore arm. No standing in a long line to get it either.
This is the vision that researchers at Stanford hope to achieve with a new tetanus vaccine derived from a bacterial species that’s found on the skins of virtually all human beings; one that’s largely harmless to us, yet nevertheless will trigger a ferocious antibody response if it breaches the skin barrier or gets inside the bloodstream.
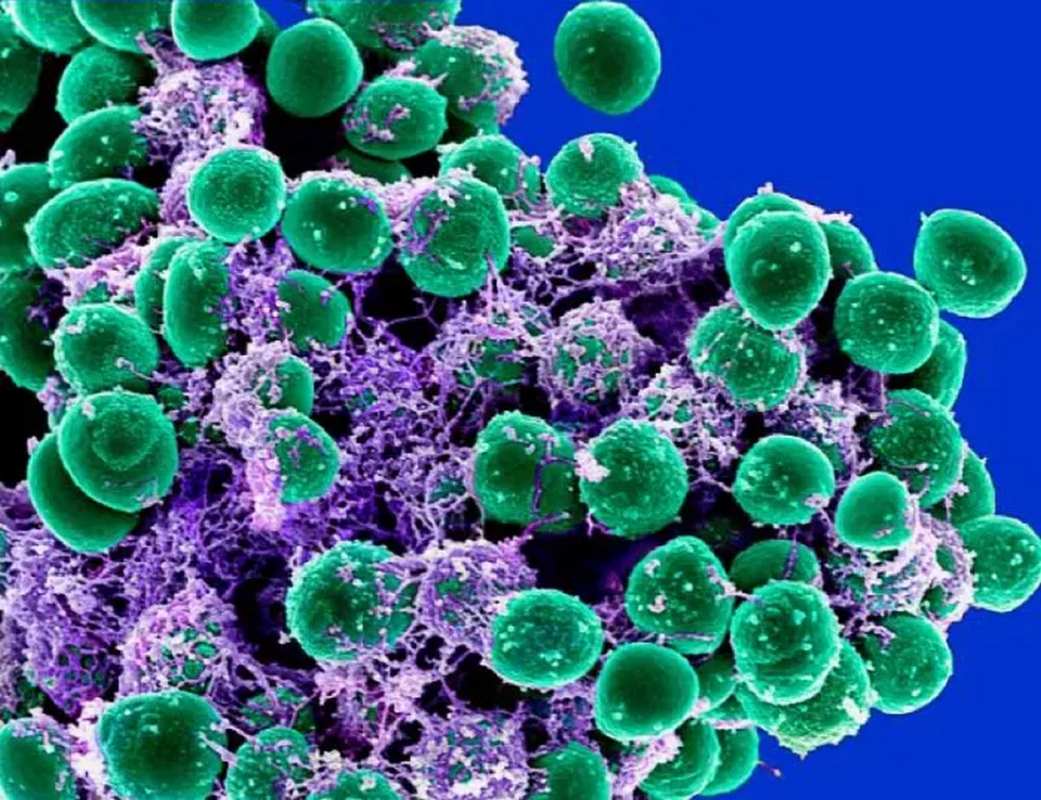
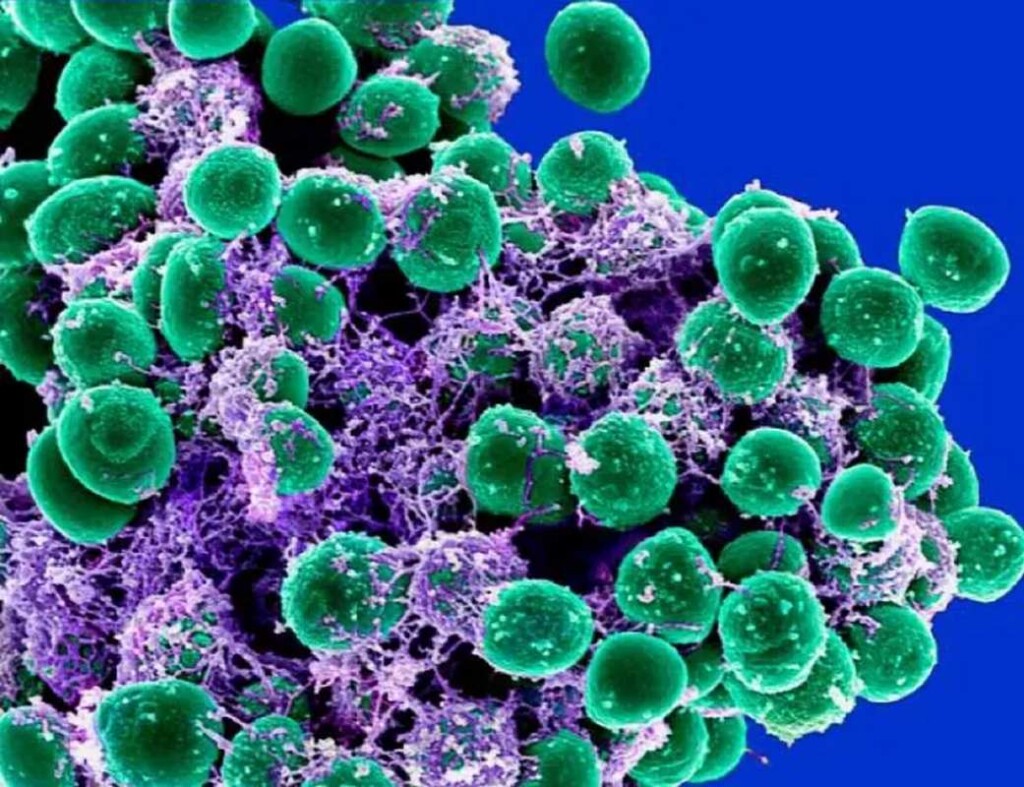
A team of scientists led by the Standford Ph.D. in bioengineering Dr. Michael Fischbach hypothesized that Staphylococcus epidermidis, the harmless and ubiquitous bacterium, could be used as a delivery mechanism for the pathogen in a vaccine.
During experiments, Fischbach found that when the S. epidermidis bacteria were engineered to contain a small genetic trace of the tetanus bacteria, the immune system targeted it just as ferociously as before, while also resulting in a separate immune response to the tetanus gene of the kind one would expect from a vaccine.
The team learned through further examination of S. epidermidis that it naturally produces a large protein called Aap. This tree-shaped molecule is five times larger than normal proteins, and so large its ‘branches’ protrude from the cell wall. Fischbach and his team believe that this is the reason why the immune system’s response to this microbe is so robust: immune cells on our skin and hair follicles can study it even without coming in direct contact with it.
Mice, which have no native colonization of S. epidermidis, were found to have greater-than-vaccine level immune responses to this bug after it was swabbed directly onto their fur.
Fischbach and his team determined that this could be the basis for a topical vaccine, one in which the bacteria is engineered to carry the genetic material of humanity’s most dangerous diseases. Further tests carried out on the mice found that application of S. epidermidis engineered to carry tetanus generated enough antibodies to protect mice from six times the lethal dose of tetanus toxin—a truly astonishing discovery.
MORE EXPERIMENTAL VACCINES: Hate Needles? Future Vaccines Could be Delivered by a Gentle Puff of Air
“We think this will work for viruses, bacteria, fungi, and one-celled parasites,” Fischbach told Stanford University press. “Most vaccines have ingredients that stimulate an inflammatory response and make you feel a little sick. These bugs don’t do that. We expect that you wouldn’t experience any inflammation at all.”
Most vaccines given to humans come in two forms, a live vaccine or a dead vaccine. Live vaccines contain the real thing, and side effects of the kind one would expect from an infection are not uncommon. In dead vaccines, the virus or bacterium can’t replicate. Antibody response to a dead vaccine is enhanced in modern vaccines by the presence of an ‘adjuvant’—like aluminum salts.
PERSONALIZED CANCER VACCINES: Hope for Patients with Aggressive Breast Cancer: Vaccine Trial Results in 88% Survival Rate After 3 Years
Aluminum is a toxic heavy metal like cadmium or lead, and its identification when found with the virus causes the immune system to respond much more seriously. The brilliance of what Fischbach called the “plug-and-play” vaccine cream developed in his lab is that the adjuvant is a harmless skin bacteria that already exists on the skin and hair of nearly every human on the planet.
Fischbach believes trials for the cream will commence in humans within 2 to 3 years.
SHARE This Breakthrough On Topical Vaccine Application With Your Friends…